GAVE Treatment Modalities
Ablation therapies are typically first line treatments in GAVE. However, gastroenterologists may try different options, depending on the patient and the progression of the disease.
Lifestyle Changes and Nutrition
Before any invasive treatments, patients should first try lifestyle and nutrition changes. They should avoid NSAIDS and alcohol and take iron supplement to address the anemia. These changes can decrease the need for transfusions, however, lifestyle changes lack a long term solution for chronic patients and the patient most often will ultimately need a transfusion.
Pharmaceutical
Evidence for pharmacological therapy with Tranexamic Acid and steroids is limited, stemming from case reports only. These have been used if endoscopic measures have failed to stop chronic blood loss. The oral medication Tranexamic Acid stops the bleeding through an antifibrinolytic mechanism, but is fraught with limitations and complications. Steroids are used to control the symptoms of scleroderma, however some of the side effects of steroid usage include gynecomastia, menorrhagia, steroid-induced diabetes mellitus and Cushing-like illness.
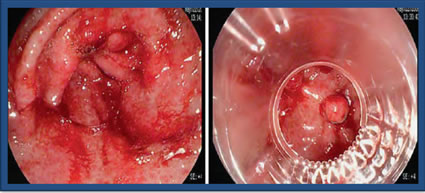
Endoscopic Band Ligation
Endoscopic Band Ligation (EBL) is performed endoscopically by placing small rubber bands around the bleeding areas. This is typically used for esophageal variceal bleeding and sometimes used in the setting of non-variceal bleeding, such as GAVE. EBL requires fewer sessions when compared to Argon Plasma Coagulation (APC) and can be a salvage after APC failure, however, it can lead to complications, such as epigastric pain, ulcers and perforation. Currently, there is limited data on the success of EBL. This picture represents GAVE before and while undergoing ligation with 5 bands.
Surgical Antrectomy
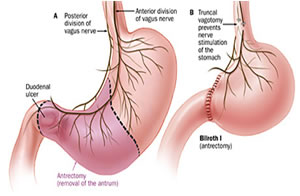 Antrectomy is the surgical resection or removal of the gastric antrum. It is an invasive procedure associated with significant complications, such as ulcers, diarrhea, dumping syndrome and malnutrition. The surgical antrectomy should be reserved for unresponsive cases as it is associated with a high mortality rate of 5%-10%.. Antrectomy is usually reserved for patients with recurrent bleeding or other conditions such as malignancy, perforation, or obstruction.
Antrectomy is the surgical resection or removal of the gastric antrum. It is an invasive procedure associated with significant complications, such as ulcers, diarrhea, dumping syndrome and malnutrition. The surgical antrectomy should be reserved for unresponsive cases as it is associated with a high mortality rate of 5%-10%.. Antrectomy is usually reserved for patients with recurrent bleeding or other conditions such as malignancy, perforation, or obstruction.
Endoscopic
The initial management of GAVE patients often includes an endoscopic intervention, which typically has been argon plasma coagulation (APC); however, despite repeat APC, some patients require frequent transfusions.
Even though these therapies are relatively inexpensive, they often need to be repeated over the course of several visits to achieve hemostasis. Other therapies include Nd:YAG (neodymium: yttrium-aluminum-garnet) laser coagulation, which has fallen out of favor due to the higher risk of perforation given the deeper thermal effect.
Endoscopic sclerotherapy, the use of a heater probe, and cryo-therapy (freezing) for treatment of GAVE have also been described in the literature. These are similar in the same therapeutic response as APC. Complications can include epigastric pain, ulcers and perforations (up to 24%).
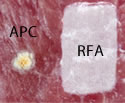
Endoscopic RFA
Radiofrequency Ablation (RFA) provides a controlled depth of ablation that limits the coagulative effect to a depth of 0.5-1mm. Blood vessels associated with bleeding for GAVE are thought to be confined to the mucosal layer within this targeted depth of ablation. The RFA electrodes come in a few sizes. The physician determines the size of the electrode based on the extent of the affected area. The electrode surface area and high-power density allows for rapid treatment of a broad area of affected tissue (< 1 second per application). This represents the largest treatment area of any thermo-coagulative device indicated for GAVE. Notice the picture comparing APC to focal ablation.


Using RFA, with this larger electrode, hemostasis is achieved through the delivery of RF energy combined with a tamponade (the stoppage of the blood flow to an organ or a part of the body by pressure) effect from the mechanical pressure of the bipolar electrode.
In a recent webinar, Dr. Scott Corbett stated that, based on his own experience and opinion, he only "does one session to achieve hemostasis, compared to 3 times with APC. Even though APC is less expensive, the cost of the procedures goes up when you add in the multiple times a patient comes in for the procedure (anesthesia, staff, etc.)."
There are promising results with over 65 peer-reviewed publications describing the safety and efficacy of ablation with the RFA System in the GI tract; although the studies on GAVE are not as voluminous, they are forthcoming with more adoption of the use of RFA for GAVE. Dr. Goss and Wallace conducted a 6 patient GAVE case series and reported fewer required treatment sessions (1.7) to increase hemoglobin levels (from 8.6 to 10.2 g/dl) and reduce transfusion dependency at 2-month mean follow-up. Four of six patients had previously failed treatment with APC.
It is widely believed that GAVE is under-recognized and that it is often misdiagnosed as antral gastritis. Tsai et al. reported an average latency of five years before antral vascular ectasias are identified as the origin of GI blood loss. Therefore, it is important to keep in mind the possibility of GAVE in the differential diagnosis of chronic occult upper GI bleeding in a patient with iron deficiency anemia that is resistant to conventional treatment.
Next Page: Radiation Proctitis